Out of the palate


Introduction
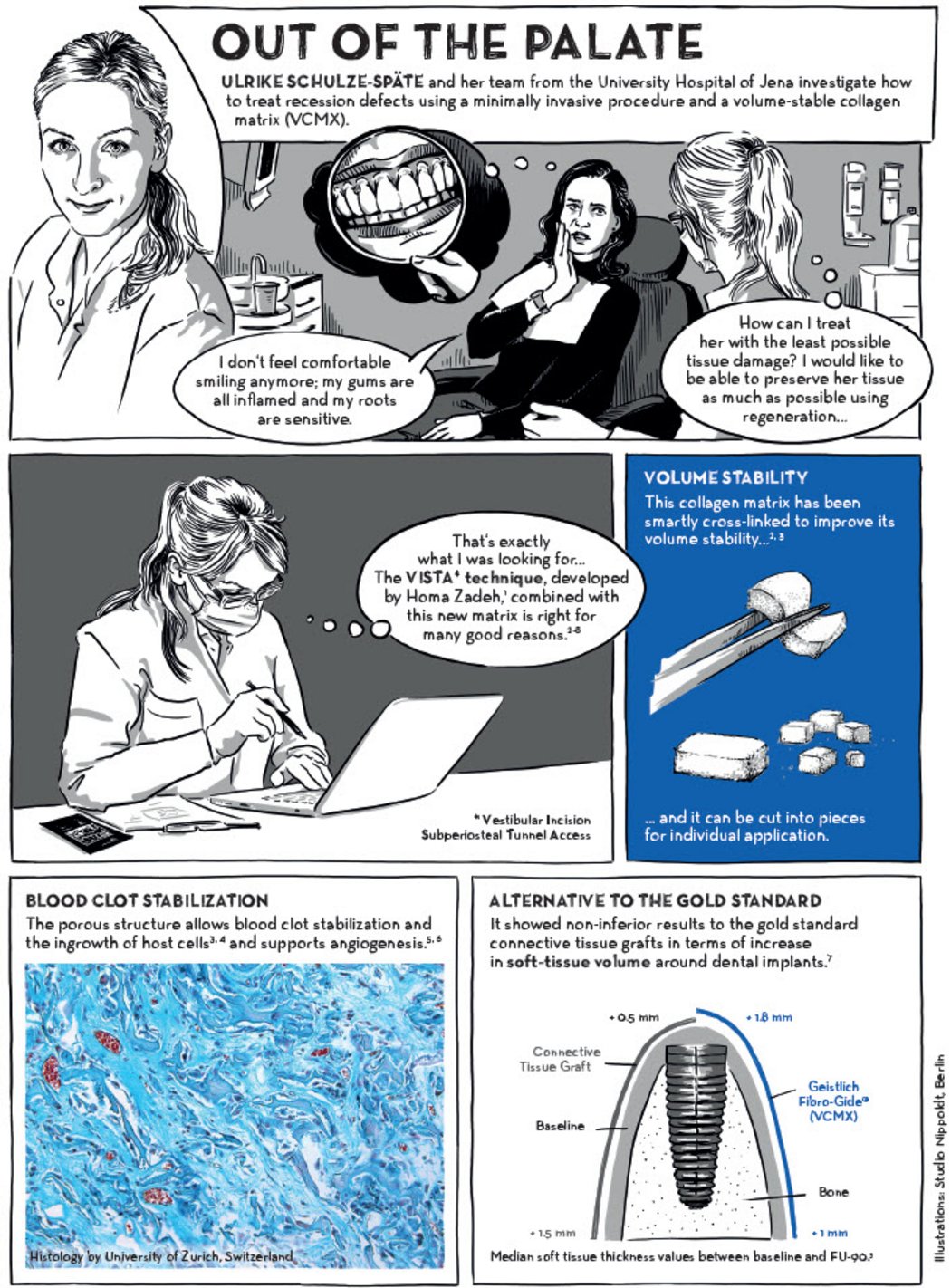
Gingival recession is a common dental concern that can lead to root sensitivity, inflammation, and aesthetic issues. Traditionally, soft tissue grafting has involved autologous tissue harvesting, which can increase surgical trauma and patient discomfort. However, Ulrike Schulze-Späte and her team from the University Hospital of Jena have introduced a minimally invasive approach using the VISTA-X technique combined with Geistlich Fibro-Gide®, a volume-stable collagen matrix.
This innovative approach reduces the need for palatal tissue harvesting, minimises surgical trauma, and supports predictable soft tissue regeneration. This article explores how Geistlich Fibro-Gide® contributes to gingival recession treatment by providing volume stability, blood clot stabilisation, and an alternative to traditional connective tissue grafts.
Minimally Invasive Approach to Gingival Recession Treatment
The Challenges of Gingival Recession
Gingival recession affects both function and aesthetics, leading to:
- Increased root sensitivity
- Inflammation and discomfort
- Aesthetic concerns impacting patient confidence
The VISTA-X Technique: A Game Changer
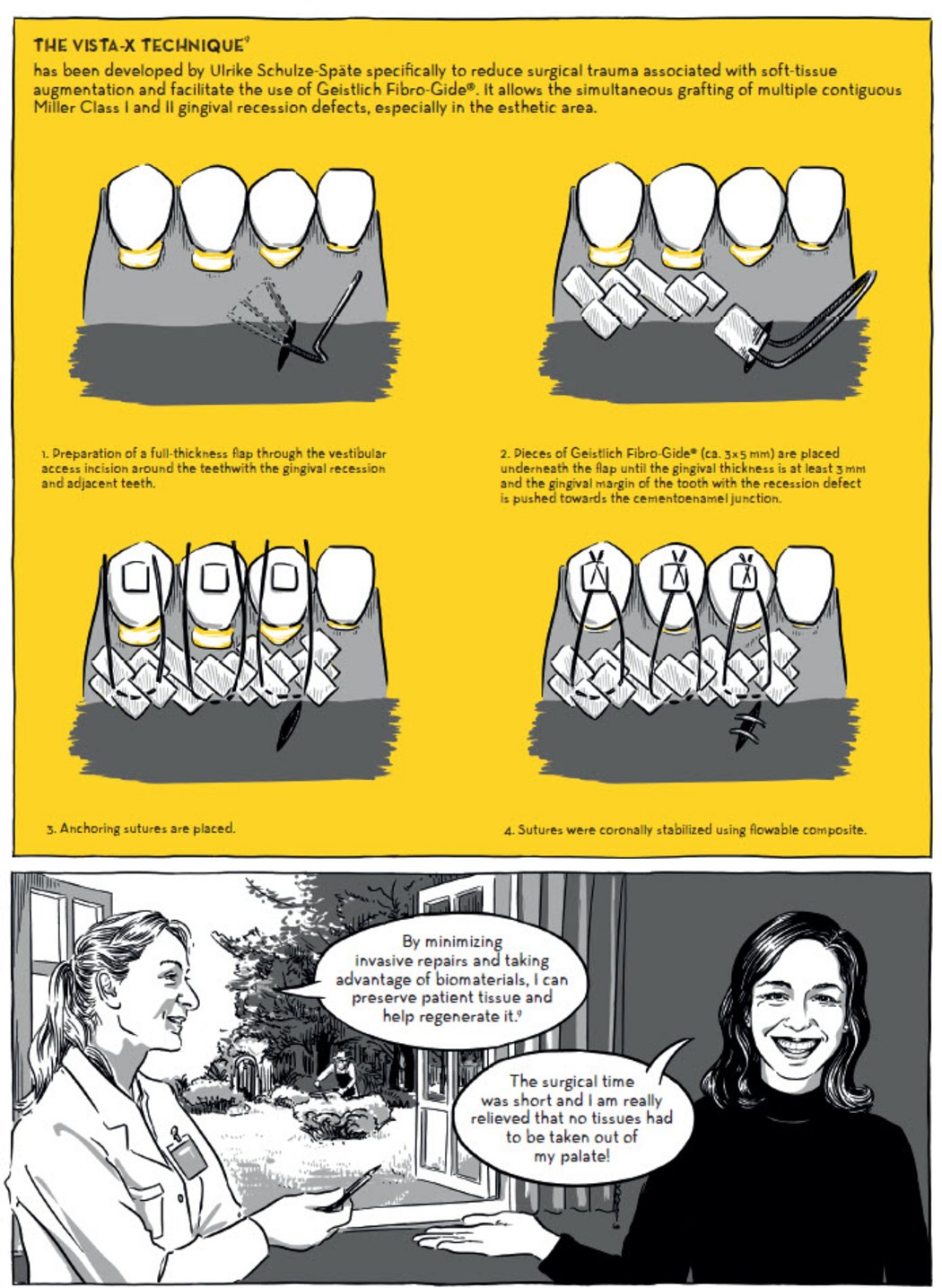
The VISTA-X technique, developed by Ulrike Schulze-Späte, is designed to:
- Reduce surgical trauma
- Preserve soft tissue without palatal grafting
- Allow simultaneous grafting of multiple recession defects
Step-by-Step Guide to VISTA-X with Geistlich Fibro-Gide®
1. Creating a Minimally Invasive Flap
- A full-thickness flap is prepared through a vestibular incision around the teeth affected by gingival recession.
2. Inserting Geistlich Fibro-Gide® for Soft-Tissue Augmentation
- Geistlich Fibro-Gide® is cut into 3 × 15 mm pieces and positioned underneath the flap.
- The gingival thickness must reach at least 3 mm, and the gingival margin is carefully repositioned towards the cementoenamel junction.
3. Anchoring Sutures for Stability
- The flap is secured with anchoring sutures.
4. Final Stabilisation Using Flowable Composite
- To enhance stability, sutures are coronally stabilised using flowable composite.
Why Geistlich Fibro-Gide®?
1. Volume Stability Without Palatal Tissue Harvesting
Unlike traditional connective tissue grafts, Geistlich Fibro-Gide® is a volume-stable collagen matrix that:
- Maintains its structural integrity over time.
- Can be cut to size, allowing for a customised approach for each patient.
2. Blood Clot Stabilization & Angiogenesis Support
The matrix’s porous structure facilitates:
- Blood clot stabilization
- Host cell ingrowth
- Angiogenesis (new blood vessel formation)
(Source: Histology by the University of Zurich, Switzerland.)
3. Alternative to the Gold Standard Connective Tissue Graft
- Studies show non-inferior results compared to autologous connective tissue grafts in soft tissue volume increase around dental implants.
(Source: Median soft tissue thickness values between baseline and FU-90.)
Patient & Clinician Testimonials
Clinician’s Perspective:
"By minimising invasive repairs and taking advantage of biomaterials, I can preserve patient tissue and help regenerate it!"
Patient’s Experience:
"The surgical time was short, and I am really relieved that no tissue had to be taken out of my palate!"
Conclusion: A New Standard for Gingival Recession Treatment
The combination of VISTA-X and Geistlich Fibro-Gide® is setting a new standard in periodontal plastic surgery. This approach minimises patient discomfort, eliminates the need for palatal tissue harvesting, and provides predictable soft tissue regeneration.
For clinicians looking to enhance their soft tissue augmentation procedures, this method offers a proven, effective, and minimally invasive alternative to traditional connective tissue grafts.
References:
- Zadeh HH. Int J Periodontics Restorative Dent. 2011; 31(6):653-60. (Clinical study)
- Instructions for Use. Geistlich Fibro-Gide®. Geistlich Pharma AG, Wolhusen, Switzerland.
- Data on file. Geistlich Pharma AG, Wolhusen, Switzerland (Pre-clinical study).
- Thoma DS, et al.: Clin Oral Implants Res. 2012; 23(12): 1333–9. (Pre-clinical study)
- Thoma DS, et al.: J Clin Periodontol. 2016; 43(10): 874–85. (Clinical study).
- Thoma DS, et al.: Clin Oral Implants Res. 2015; 26(3): 263–70. (Pre-clinical study).
- Zeltner M, et al.: J Clin Periodontol. 2017; 44(4): 446–453. (Clinical study)
- Huber S, et al.: J Clin Periodontol. 2018; 45(4):504-512. (Clinical study)
- Schulze-Späte U, Lee CT. Int J Periodontics Restorative Dent. 2019; 39(5):e181-e187. (Clinical study)

Dr. Ulrike Schulze-Spaete
PD Dr Ulrike Schulze-Späte, DDS, CAGS
Head of the section and specialist in periodontology (American Board of Periodontology)