Periodontal disease and systemic health

Understanding the Systemic Impact of Periodontitis
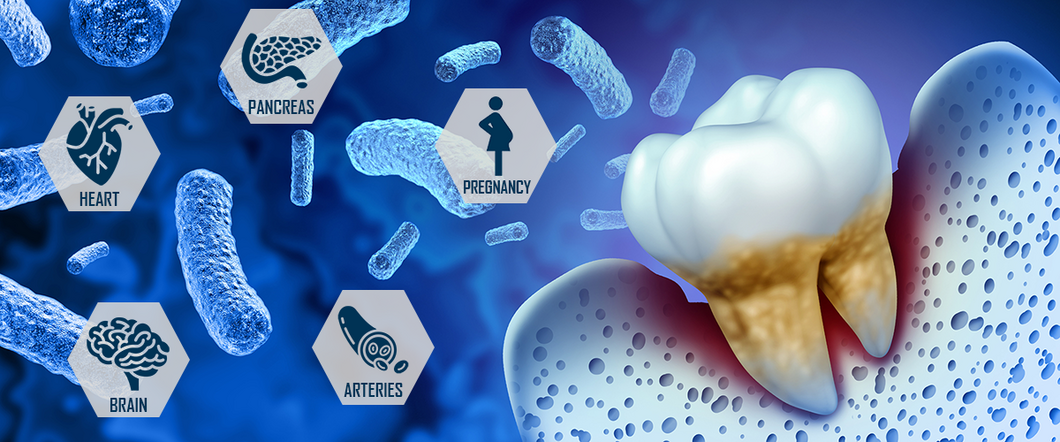
As dental professionals, we know that periodontal disease is more than a localized oral issue. But how often do we consider its broader implications for systemic health? Growing evidence links periodontal disease to cardiovascular conditions1-6, diabetes7-9, Alzheimer’s disease10 and even pregnancy complications11, 12.
It's time to integrate the systemic relationship between oral health and overall well-being into our patient communications and clinical approach.
A Global Burden with Systemic Reach
Severe periodontitis affects over 500 million people globally, making it the sixth most prevalent health condition worldwide13-15. Including milder forms, nearly half of all adults are affected5. This is not just a statistic; it's a public health concern. Chronic gum inflammation serves as a persistent source of bacteria and inflammatory mediators that could enter the bloodstream and influence systemic health1-4,6.
Periodontitis and Diabetes
One of the most well-established connections of periodontitis to systemic health is diabetes. The relationship is bidirectional: diabetes increases susceptibility to gum diseases, and untreated periodontitis can worsen glycemic control7-9.
The Heart–Gum Association
Cardiovascular disease (CVD) remains the leading cause of death globally, and periodontitis is increasingly recognized as a contributing risk factor. A consensus report by the European Federation of Periodontology (EFP) and the World Heart Federation concluded that periodontitis increases the risk of atherosclerotic cardiovascular disease (ASCVD), including heart attacks and strokes5.
Periodontitis and Heart Disease
The 'Periodontitis and Its Relation to Coronary Artery Disease' (PAROKRANK) study in Sweden reported an association between periodontitis and the first myocardial infarction/ first heart attack1-3.
The 10 years follow-up of the PAROKRANK study found that individuals with periodontitis had about a 28% higher risk of a first heart attack, even after adjusting for smoking and other risk factors4.
Periodontitis and Stroke
The ARIC study in the U.S. reported that people with severe periodontitis had more than double the risk of ischemic stroke5.
Periodontitis and Peripheral Artery Disease
Studies from NHANES and KoGES show that advanced gum disease is associated with a twofold increase in peripheral artery disease5.
Periodontitis and Systemic Inflammation
The plausible biological connection between periodontitis and various systemic diseases is inflammation. Severe periodontitis can trigger low-grade chronic inflammation with far-reaching systemic impact6. Recent research shows that the oral microbiome in the gums of patients with severe periodontitis is significantly different than those in patients with mild periodontitis, which is associated with systemic inflammation6. This critical factor could be the link of oral health issues to cardiovascular disease6, stroke5, and peripheral artery disease5.
Trained immunity and inflammation
Recent research from Radboud University investigated whether periodontitis may contribute to cardiovascular disease through a process called trained immunity. This refers to a form of “memory” in immune cells like monocytes, which become “more reactive” after exposure to bacteria such as P. gingivalis. This effect was demonstrated in an in vitro study. While not observed in circulating immune cells in patients with periodontitis, “reactive” immune cells were visualized in gums and bone marrow tissues by PET scans. This suggests that trained immunity might play a role and requires further investigation16.
Link of periodontitis and neurodegenerative diseases
Reviews suggest that periodontitis may increase the risk of Alzheimer’s disease by up to five times. The underlying mechanism is thought to be chronic inflammation, which may trigger neuroinflammation through immune, humoral, and neural pathways. Since periodontitis is treatable, it may represent a modifiable risk factor for slowing cognitive decline and neurodegeneration10.
Gingivitis and Periodontitis during Pregnancy
Hormonal changes throughout a woman’s life, such as puberty, pregnancy, and menopause can significantly affect periodontal health. During pregnancy, 60–75% of women develop gingivitis17, and those with periodontitis face a twofold increased risk of preterm birth12. Periodontal pathogens have even been detected in placental tissues, suggesting a direct microbial link11.
Treating Periodontitis: Systemic Benefits
So, what happens when we treat periodontitis? The benefits extend beyond the mouth:
- Reduced Inflammation: Periodontal therapy lowers systemic markers and improves endothelial function, which is beneficial for cardiovascular health18-23.
- Better Diabetic Control: Treating gum disease can lead to improvements in blood sugar levels7-9.
- Lower Healthcare Costs: A US insurance study found that patients with diabetes and/or heart disease who received regular dental care had significantly lower medical costs and fewer hospitalizations24.
- Improved Quality of Life: Beyond clinical metrics, patients report better chewing function, self-esteem, and overall well-being after periodontal treatment25,26.
A Call to Action for Dental Professionals
As dental professionals, we are uniquely positioned to influence both oral and systemic health. The evidence is increasing that periodontitis is not an isolated condition. It is suspected to be a modifiable risk factor for multiple systemic diseases. By prioritizing periodontal diagnostics and care, we’re not just preserving smiles. We are potentially taking preventive measures for serious systemic diseases, supporting healthy pregnancies, and improving chronic disease outcomes.
Explore Treatment Solutions
Let’s continue to educate our patients and ourselves about the far-reaching impact of oral health.
For those looking to integrate regenerative solutions into their periodontal treatment protocols, explore how Geistlich’s evidence-based products can support your clinical outcomes: Geistlich Periodontal Treatment Solutions
References
- Rydén L, et al.: Circulation 2016; 133(6): 576–83. (clinical study)
- Norhammar A, et al.: Diabetes Care 2019; 42(8):1504–11. (clinical study)
- Nordendahl E, et al.: J Dent Res 2018; 97(10): 1114–21. (clinical study)
- Norhammar A, et al.: J Clin Periodontol 2025; 52(1): 16–23. (clinical study)
- Sanz M, et al.: J Clin Periodontol 2020; 47(3): 268–88. (consensus report)
- Plachokova AS, et al.: Int J Mol Sci. 2021 May 30;22(11):5876. (clinical study)
- American Academy of Periodontology: Gum Health and Diabetes, accessed July 24, 2025. (web article)
- Demmer RT, et al.: Diabetes Care 2012; 35(11): 2235–42. (clinical study)
- Genco RJ, et al.: Periodontol 2000 2020; 83(1): 59–65. (review)
- Plachokova AS, et al.: Int J Mol Sci. 2024 Apr 19;25(8):4504. (review)
- European Federation of Periodontology: Women and oral health: views from periodontology and gynaecology, accessed July 14, 2025. (web article)
- Manrique-Corredor, et al.: Community Dent Oral Epidemiol 2019; 47(3): 243–51. (systematic review)
- Kassebaum NJ, et al.: J Dent Res 2014; 93(11): 1045–53. (systematic review)
- Kassebaum NJ, et al.: J Dent Res 2017; 96(4): 380–387. (systematic review)
- World Health Organization: Global oral health status report, accessed July 14, 2025. (report)
- Noz M, et al.: Front Immunol 2021; 12:695227. (in vitro/in vivo study)
- European Federation of Periodontology: Gum health: a key indicator of women’s overall wellbeing., accessed July 14, 2025. (web article)
- D’Aiuto F, et al.: J Dent Res. 2005 Mar;84(3):269-73. (clinical study)
- Tonetti MS, et al.: N Engl J Med. 2007 Mar 1;356(9):911-20. (clinical study)
- Vidal F, et al.: J Periodontol. 2009 May;80(5):786-91. (clinical study)
- Isola G, et al.: J Periodontol 2024; 95: 949–62. (clinical study)
- Demmer RT, et al.: PLoS ONE 2013; 8(10): e77441. (systematic review)
- Luthra S, et al.: J Clin Periodontol. 2023 Jan;50(1):45-60. (systematic review)
- Zimmermann E: A trip to the dentist saves money, reduces likelihood of hospitalization for people with diabetes or coronary artery disease. Mayo Clinic News Network, accessed July 14, 2025. (web article)
- Baiju RM, et al.: J Clin Diagn Res. 2017 Aug;11(8):ZC14-ZC19. (systematic review)
- Sischo L, Broder HL: J Dent Res. 2011 Nov;90(11):1264-70. (review)

Dr. Adelina S. Plachokova, DDS, PhD
Assistant Professor in Periodontology;
Chair of the Education Committee Radboud University Medical Center, Nijmegen, The Netherlands;
Certified Periodontist, Dutch Society of Periodontology

